It’s hard to see the horizon when you’re fighting to keep your head above water.
That’s where AEC firms, interviewed in late March and through April, say most of their clients were when it came to infection control during the pandemic. No one was thinking long term, and immediate actions were “small-bore tactical moves” like installing handwashing sinks, touchless point-of-sale at retail, and enforcing social distancing, says David Levo, Principal and Higher Ed Practice Leader with Perkins Eastman.
But uncertainties about the virus, including the possibility of a second wave this fall or winter in the U.S. if a vaccine isn’t found by then, left businesses grappling for answers: what can and should they do, and what could they afford?
“Our clients will need to evaluate cleaning regimens,” says Steve Turckes, FAIA, LEED AP, Principal and Global K-12 Market Sector Practice Leader with Perkins and Will. “I strongly suspect that infection control will extend to all parts of the building.”
Perkins and Will’s higher education clients with student living might need to consider quarantine measures, laying out dorms with double-loaded corridors that mimic hospital floors, increasing electrical capacity, and upgrading ventilation systems for medical use, says David Damon, AIA, LEED AP, Principal and Higher Education Practice Leader with Perkins and Will.
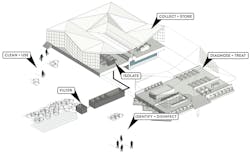
A slew of AEC firms formed response and recovery task forces during the pandemic to help guide their clients’ decisions. A remarkable number of firms—including AECOM, Leo A Daly, Robins & Morton, HOK, HDR, Gensler, NBBJ, HGA, The Boldt Company, Hensel Phelps, and Walsh Construction—stepped up with ready-to-go concepts to address hospitals’ surge capacity shortcomings by converting existing buildings like hotels, schools, dorms, gymnasiums, and convention centers that were vacated during virus lockdowns in their markets.
The health crisis also presented firms the opportunity to reiterate the virtues of modular design. “There’s been a lot of conversation about modular,” says Solvei Neiger, AIA, ACHA, Partner and Healthcare Practice Leader with ZGF Architects, which during the pandemic was working with contractors on a modular healthcare facility in Portland, Ore.
COVID-19 brings attention to airflow
Nolan Rome, WSP USA’s Senior Vice President and Healthcare Practice Leader in Dallas, observed that infection control in buildings “is about air containment as much as PPEs.” Many firms would agree, and say they’ve been challenging their clients for years to invest in advanced HVAC and ventilation systems to improve their buildings’ air quality and germ patrol.
In their efforts to stem the spread of infection in their new projects, developers might be more open to passive strategies “that challenge the status quo” about ventilation, suggests Deborah Wingler, PhD, EDAC, Vice President and Health Research Lead with HKS.
Measuring results will also be key. DLR Group has been researching air quality since 2014 through various pilot programs that encompassed all of its offices worldwide and the 4.2 million-sf Merchandise Mart in Chicago. Its latest pilot, with the General Services Administration, started with a redesign of three floors of GSA’s Chicago office. GSA had been using an air-quality scorecard that didn’t include the building’s HVAC system. So the pilot set out to learn what GSA does when it designs a space, to overhaul the scorecard to include measurements for ventilation, air quality, and comfort, and to share the data via public review.
The scorecard is now “crowdsourced,” and “has changed how GSA evaluates design,” says Shona O’Dea, BEMP, RESET AP, WELL AP, LEED AP, Senior Associate and Building Performance Analyst with DLR Group.
Its work in other countries that were hit by infectious diseases has informed the designs that MASS Design Group performs domestically. These include the Cholera Treatment Center in Port-Au-Prince, Haiti, whose layout facilitates patient screening and isolation.
In a recent paper about how HVAC systems in schools should address COVID-19, Fanning Howey’s Timothy Lehman, PE, LEED AP, Mechanical Discipline Director and Senior Associate; and Mark Hopf, PE, CEM, Mechanical Engineer, cited recent ASHRAE guidance that advocates for supplying cleaner air to susceptible occupants, containing contaminated air or exhausting it to the outdoors, diluting the air in the space with clean and filtered outdoor air, and cleaning the air within the room.
The authors also urged that building maintenance be expanded to more extensive use of ultraviolet lamps to purify HVAC systems.
“HVAC is a big piece of this,” says Jim Henry, AIA, Senior Vice President and Healthcare Director with CallisonRTKL. “We need to control the flow of diseases that we don’t even know about.” Henry recently was on a conference call with the firm’s Senior Living Practice lead, “and we talked about the same thing: fusing health, wellness, and care.”
Design and behaviors must coincide
Not every firm’s expert expects game-changing modifications, either in the work they do or the finished product, in the wake of the pandemic. Design can only do so much, and our experts assert that people’s behavior will be the main determinant of the relative impact of any future viral events.
Fiona Cousins, PE, LEED Fellow, Principal and Digital Services Leader with Arup, points out that “to many people’s surprise” most existing buildings, including hospitals, are not built for infection control, “and it would be very difficult, expensive, and probably unnecessary to retrofit buildings to achieve this.”
Matt Needham, Principal and Regional Aviation−Transportation Leader with HOK, doesn’t anticipate significant structural changes in airports to thwart infection. But higher travel fees might be in the offing, he says, to defray the cost of adding technology for such upgrades as automation improvements in touchless baggage processing and rigorous passenger screening that includes the use of “fever sensors.”
So, what will and should be done, and where do AEC firms fit in, when it comes to infection control?
“There needs to be a general rethinking about the requirements of infection control for all typologies,” asserts David Tepper, AIA, Principal and Healthcare Practice Leader with Ennead Architects. Flexibility and robust infrastructures are the most important factors for healthcare facilities, says Tepper.
ALSO SEE: The 'Six Feet Office' and other infection control strategies for the workplace
The workplace, post COVID-19, is being viewed as “the first line of defense in preventing the spread of infectious germs,” says J. Kevin Heinly, AIA, LEED AP, Principal and Managing Director of Gensler’s San Diego office. Learn how Heinly and other workplace design experts are preparing their clients for the return to work in this BD+C exclusive report.
TPG Architecture’s recommendations to its hospitality clients—whose properties took major business losses during the pandemic—are framed in three stages: now, near, and future, says Shay Lam, IIDA, Managing Executive and Studio Creative Director. For “now,” hotels should focus on pragmatic changes like reducing density in public areas. “We are also adding clearer signage for protocols such as distancing,” says Lam.
For the “near,” TPG is looking at integrating touchless or voice technology. Lam also believes it is critical for hotels to maintain stringent, visible cleaning cycles, and to find ways to sanitize commonly used areas.
The “future” presents opportunities to rethink hospitality, says Lam. That might include changing the size ratio of public spaces vs. guest rooms. Employee uniforms, including branded face masks and hats, must be cleaned and sanitized daily. “And, of course, lots of handwashing,” says Lam.
During the pandemic, outpatient clinics went dormant because they weren’t set up to treat infected patients. Gensler saw this as symptomatic of a healthcare system unprepared to handle surges better during critical periods.
“We believe more than ever that widely distributed health networks can change access to care and the shape of cities,” wrote Gensler’s Global Health & Wellness Practice Leaders Randy Guillot, James Crispano, and Scot Larimar.
Gensler advocates for advance planning to be able to get temporary hospitals up and running faster, more multifunctional hospital rooms and clinics, putting support spaces like garages to better use as testing sites, reactivating former patient care spaces, and expanding modular design and construction for flexibility.
Social distancing in the age of coVID-19
Pre-vaccine, any building with a lobby or reception area must consider its responsibilities to both tenants and visitors. “Do they provide PPEs and sanitizers? How do they take people’s temperatures? How are the restrooms set up?” asks Sam Nunes, AIA, LEED AP, Founding Partner with WRNS Studio.
Construction jobsites are also uncharted waters for infection control. Clark Construction was among the GCs that implemented a COVID-19 management plan that reinforces the importance of physical and social distancing, hand hygiene, and “respiratory etiquette.” Clark’s plan includes educating its workforce about the virus’ symptoms; requiring ill workers and high-risk individuals to stay home; cleaning frequently touched surfaces, portable toilets, and shared tools; and even deploying a rotational telework schedule for management staff.
Turner Construction’s infection control plan is similar to Clark’s, and encourages workers to proactively self-check their temperatures before coming to the office or work. Turner also implemented temperature-screening measures that include on-site scanning stations to detect infection and minimize a virus’ spreading.
Physical distancing on a jobsite will require other operational changes. “As long as infection control measures prohibit or limit site visits and in-person meetings, point-cloud technology will be integral to promoting safety and maintaining a project’s design schedule,” wrote Andrew Graham, AIA, a Design Architect with Leo A Daly, and Jason Dittrich, Director of Business Development and Marketing with Mueller Associates, an ME firm, in a report.
Graham and Dittrich said that by using data collected from laser scans, “we’ve been able to cut down in-person visits by between 70% and 80%.”
Heeding infection control experts
The coronavirus exposed the critical need for facts and science to guide infection control actions. And some AEC firms were taken to task by competitors and colleagues for being too eager about predicting the future, when so little was actually known about the virus and how it spread.
AEC firms that trade on their expertise often do so based on their relationships with outside experts who, moving forward, could become more important advisors in the search for answers to complex public health questions.
“We believe in collaborating with smart people,” says WRNS Studio’s Nunes, who adds that he might start looking for a healthcare scientist to enhance his firm’s stable of consultants.
ALSO SEE: How the coronavirus pandemic could change the built environment
“We’ll never look at any kind of space the same way again,” says Terri Zborowsky, PhD, EDAC, Evidence-based Design Researcher with HGA. That firm’s co-designing process now includes healthcare professionals on such topics as cleanliness and respite. “Those voices are at the table so we can make the next design decisions.”
Michael Compton, AIA, ACHA, EDAC, Healthcare Design Leader with RS&H, a national AE firm, says that his people regularly consult with healthcare clients’ infection control “champions” about design, construction, and operations. “They establish the baseline,” says Compton. His firm also asks clients to participate in research, such as a recent “foam-in/foam-out” study to determine where antibacterial scrubbing should occur in a hospital room. That study concluded that the sink should be located inside of a patient’s curtain area.
“You have to understand a client’s standards” and be able to cite research that might improve best practices, says Compton. Informed persuasion is key, says Compton, who is skeptical that building owners will react to future crisis events in meaningful ways unless they are encouraged or required to do so. “I feel the adoption of any preventive measures will take some time.”