When evidence-based design collides with conventional wisdom, the outcome will sometimes be disruptive.
Take, for example, the generally accepted advantages in patient care and observation related to decentralizing nurses’ stations in hospitals, which is becoming standard practice for healthcare clients and their AEC partners.
A recent evaluation of a renovated Missouri hospital, conducted by University of Kansas faculty members, raised questions about the impact of decentralization on patient satisfaction and the communication among nursing teams within the facility.
The St. Louis-based architectural firm Lawrence Group retained the Institute for Health + Wellness Design (IHWD) at KU’s School of Architecture, Design, and Planning to provide a third-party review of the firm’s 2014 remodeling of the orthopedic unit at SSM St. Mary’s Hospital in Jefferson City. That healthcare system was about to embark on an expansion of its St. Joseph Hospital West in Lake St. Louis.
Lawrence Group is an affiliate member of IHWD.
The Institute assessed the unit using an evidence-based design checklist developed by the nonprofit Center for Health Design in California. Its survey included a “space syntax” evaluation that generated a heat map, which showed how the unit’s layout might affect patient satisfaction.
“We wanted to see does moving into a new facility improve patient satisfaction scores, which is one of the most important things for hospital owners today,” said Hui Cai, Assistant Professor at KU, who with Professor Kent Spreckelmeyer and Frank Zilm, IHWD’s chairman, presented findings from the Institute’s nursing unit study at the Healthcare Design Conference 2016 in Houston last November.
The study found, perhaps not surprisingly, that the facility itself showed “statistically significant increase[s]” in scores after the renovation. But patient-quality scores mostly stayed the same, and one score—nurses’ responses to patient calls—actually dropped slightly.
The Institute hypothesizes that decentralization was the culprit, due to the physical distance and visual disconnection of decentralized nursing unit design, which necessitates that nurses must move farther to get from station to station. The Institute suggests these distances might be an impediment to interaction among nurses that might also delay responses to patients.
“This design trend needs to be further investigated before it is accepted as standard for every hospital,” said Cai. “We have to see how to modify the design to achieve balance between shorter walking distance, better patient surveillance and better staff communication and collaboration.”
This is one of the first research studies to link decentralized nurse station design with organizational performance and patient outcomes. The Institute has conducted a second phase of study to evaluate further the degree to which decentralized design affects nurses’ teamwork and patients’ perception of care. In late 2017, IHWD plans to present and publish the results of this study, which included a second hospital, the University Medical Center of Princeton at Plainsboro, N.J.
Related Stories
Healthcare Facilities | Apr 29, 2016
How improving emergency department design leads to greater hospital efficiency
Efficient ED operations result in shorter wait times, quicker diagnosis and care plans, maximum utilization of high-cost human and physical resources, and overall better patient experiences and patient satisfaction scores, writes CBRE Healthcare's Curtis Skolnick.
Healthcare Facilities | Apr 24, 2016
A symposium in New Jersey examines how a consolidating healthcare industry can better manage its excess real estate
As service providers position themselves closer to their communities, they are looking for ways to redirect non-core buildings and land for other purposes.
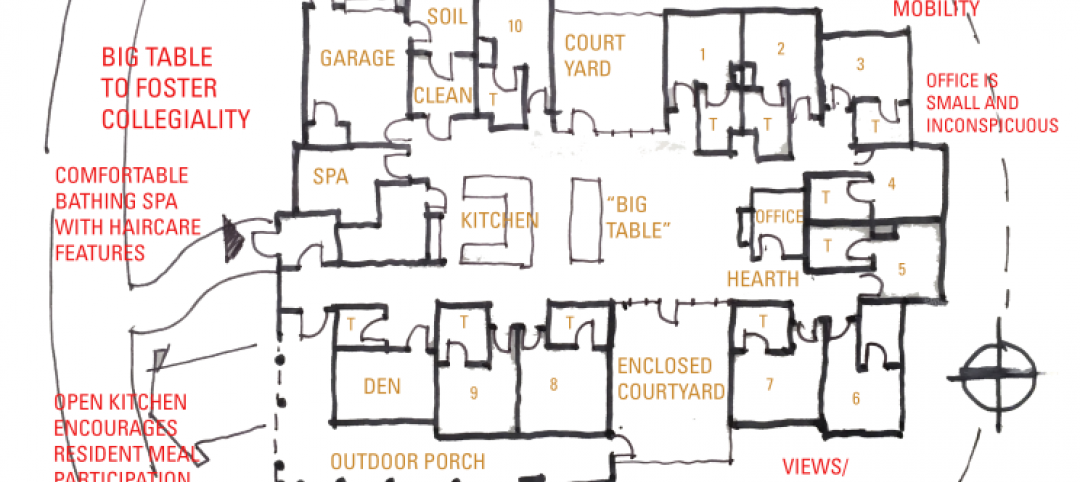
Senior Living Design | Apr 14, 2016
Creating a home for eldercare using the ‘Green House’ design concept
VOA Associates’ Douglas King offers design considerations in implementing the Green House concept in eldercare for continuing care retirement communities.
Adaptive Reuse | Apr 7, 2016
Redevelopment plan announced for Chicago’s historic Cook County Hospital
The century-old, Beaux Arts architecture-inspired hospital will transform into a mixed-use development.
Industry Research | Apr 7, 2016
CBRE provides latest insight into healthcare real estate investors’ strategies
Survey respondents are targeting smaller acquisitions, at a time when market cap rates are narrowing for different product types.
Healthcare Facilities | Mar 11, 2016
Report: Hospitals’ fossil fuel use trending downward, but electricity consumption hardly declining
A new survey from engineering firm Grumman/Butkus Associates examines electricity, fossil fuel, water/sewer, and carbon footprint of healthcare facilities.
Office Buildings | Mar 9, 2016
CBRE: Workplace wellness on the rise
As insurance premiums and deductibles continue to rise, both employees and employers are evaluating options to improve their wellbeing, writes CBRE Healthcare Managing Director Craig Beam.
Healthcare Facilities | Mar 7, 2016
Can 'active' building designs make people healthier?
The new high-performance Kaiser Permanente facility in Anne Arundel County, Md., uses the built environment to improve the overall health of its occupants, writes GS&P's Terrance Perdue.
Healthcare Facilities | Mar 4, 2016
Building a home where Alzheimer’s patients can thrive
Skanska recently completed Abe’s Garden in Nashville, Tenn., a memory care community designed to improve the lives of those affected by Alzheimer’s disease. Skanska's Senior Project Manager Jeff Elpers has more on the facility.
Healthcare Facilities | Mar 1, 2016
Christ Hospital in Cincinnati brings its joint and spine care services under one roof
The opening coincides with agreements that make this center a preferred provider for several employers with self-funded healthcare plans.