Designing learning environments to support the future of equitable health care
While the shortage of rural health care practitioners was a concern before the COVID-19 pandemic, the public health crisis has highlighted the importance of health equity in the United States and the desperate need for practitioners help meet the needs of patients in vulnerable rural communities. Approximately 20 percent of Americans live in rural areas, but barely one-tenth of physicians practice there.1 The federal government projects a shortage of over 20,000 primary care physicians in rural areas by 2025.2.
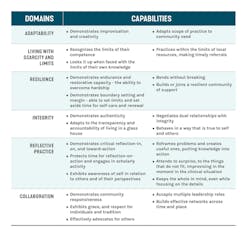
Providing care in rural and underserved areas requires providers with specific skillsets and competencies. A useful discussion of the domains and capabilities unique to rural health was developed by Randall L. Longenecker, MD and published in Family Medicine.
While not all these domains have a physical manifestation, as designers of educational facilities for the health sciences, we continually seek to design learning environments that support the unique requirements of rural health care students. Below are three themes which are important to rural health education that have guided our recent medical education projects focusing on underserved areas.
1. BUILDING DEEPER BONDS WITH THE COMMUNITY
To be successful, rural practitioners need to build strong connections with their cohorts and their communities while building a robust professional network.
A. CONNECTING TO A COHORT
- At the California University of Science and Medicine, School of Medicine (CUSM), several smaller learning spaces, known as “college rooms,” create an environment for small groups of 10-12 students to create a sense of community within their cohort and foster peer-to-peer learning.
- These “college rooms” are directly connected to generous informal spaces that encourage informal learning and socializing to foster community and build cultural competency.
- The self-contained academic building with comfortable, welcoming amenity spaces at CUSM works to create a tight-knit community to help students build a community of support that will translate into their professional network.
B. CONNECTING TO THE LOCAL COMMUNITY
By creating space for community members in the facility, the design helps students understand the unique needs of the community members they serve.
- Clinics serving the local community is central to the program at the Kansas City University School of Dental Medicine (KCU). The School of Dental Medicine will join other programs at KCU that, consistent with the traditions of osteopathic medicine, focus on primary care and whole health. Osteopathic institutions are leaders in training practitioners who are dedicated to providing care in underserved areas.
- The University of Texas Northeast School of Community and Rural Health also provides local resources including a centrally located nutrition kitchen and an adjacent flexible classroom that is available for community meetings.
C. CONNECTING TO A PROFESSIONAL NETWORK
- At CUSM, the proximity to the Arrowhead Regional Medical Center (ARMC) provides opportunities for students to engage in research with practitioners, encouraging collaboration and connecting faculty and students, while fostering critical thinking, problem solving and lifelong learning skills among both faculty and students.
- The advanced simulation environments within the CUSM School of Medicine will draw ARMC practitioners into the facility for continuing education, providing additional opportunities for interaction with students.
- The School of Community and Rural Health includes a highly visible and transparent dean's suite immediately adjacent to the common circulation areas to support faculty-student connections. Through planning and wayfinding, the School of Community and Rural Health provides connectivity with the larger context, including visibility outdoors from corridors, open vertical circulation and views through spaces.
2. ENCOURAGING ENTREPRENEURIALISM
Rural health settings often require practitioners to improvise and work with scarcity whether that is due to finances, transportation or limited access to specialists. Rural health practitioners will be well served by an entrepreneurial spirit.
- In standardized patient areas, we are seeing a focus on creating reconfigurable or adaptable settings to enable faculty and students to explore unique patient settings.
- At CUSM, open access to skills labs provides students the opportunity to practice at any time. A centrally located “Information Commons” provides access to resources and research assistance.
- At Kansas City University, faculty are accessible in and out of clinic to provide students feedback and mentoring. Similarly, at CUSM faculty workspaces are readily accessible to all students.
- Recognizing the education that takes place before and after patient encounters, our designs place an emphasis on briefing and debriefing. We are replacing generic conference rooms with additional high quality small team rooms adjacent to standardized patient areas to support these crucial learning activities.
3. FOSTERING WELLNESS AND WELL-BEING
Medical students and practitioners are under immense pressure. There is a new focus on ensuring all members of the academic community - students, residents, faculty and staff – take care of themselves to mitigate stress and model healthy behaviors in the community.
- Projects such as CUSM incorporate fitness facilities to help students meet and maintain their fitness goals. The landscaped courtyard at CUSM will introduce vegetation and create outdoor student gathering space that will take advantage of the Southern California climate.
- At Kansas City University, the master plan is consistent with osteopathic values and takes a holistic view of student demands to include academics, social and physical well-being.
- At the School of Community and Rural Health, wellness inspired the planning of the entire site. (The building shapes welcoming outdoor spaces that promote connection with nature. From an integrated fitness facility to shaded pathways that encourage students to walk and relax outside, the campus supports a variety of healthy activities.)
- Daylighting encourages a healthy mindset and the design of CUSM provides abundant natural daylight deep within the building footprint.
As architects and planners, we firmly believe that design can be transformative and that the physical environment can have an impact. When considering health sciences facilities with very unique and important goals, that can be even more critical. As you see through the themes we have shared, our work in the area of rural medicine shows that future care providers benefit from space that is transparent and connected both indoors and out; supportive of individual reflection; adaptable for new and innovative uses; team-based and interprofessional. This is an emerging area and we seek to progress our own understanding of what experiences will make a difference to future care providers. What trends do you believe will influence these educational spaces as we strive to encourage greater health equity?